Fahad Aziz, MD, FASN, WMJ Editor-in-Chief
WMJ. 2023;122(2):86-87.
A patient’s relationship with their health care provider is critical to ensuring safe and quality patient care. This relationship is based on trust and a deep understanding. Learning more about a patient than what is included in their medical history is essential to establishing a connection. Health care providers should know how to connect with their patients to provide safe, high-quality, and compassionate care. Here I describe four essential laws of connecting with patients:
- Law of Compassion
- Law of Communication
- Law of Shared Decision-Making
- Law of Hope
LAW OF COMPASSION
Before looking into “compassion,” let’s investigate sympathy and empathy and how compassion differs (Figure 1). Sympathy means understanding what the other person is feeling, while empathy is feeling what the other person is feeling. However, compassion makes us understand and feel another person’s suffering and do everything to help them come out of it.
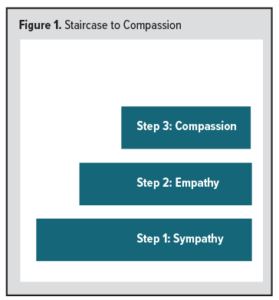 Sympathy shares similarities with compassion. Sympathy is composed of some range of feelings, while compassion, more specifically, arises in response to someone’s suffering and includes a motivation to relieve the suffering. Similarly, empathy shares a few similarities with compassion; however, it does not require action or sustain itself over an extended time.1 In other words, compassion has two components: (1) feeling someone’s suffering and (2) the ability to take action to relieve them from that suffering.2,3
Sympathy shares similarities with compassion. Sympathy is composed of some range of feelings, while compassion, more specifically, arises in response to someone’s suffering and includes a motivation to relieve the suffering. Similarly, empathy shares a few similarities with compassion; however, it does not require action or sustain itself over an extended time.1 In other words, compassion has two components: (1) feeling someone’s suffering and (2) the ability to take action to relieve them from that suffering.2,3
Several studies have shown that the compassion of health care providers is crucial for patient outcomes and satisfaction.4 A clinician’s compassion for their patients leads to a better connection between them, and patients have a faster recovery, significant autonomy, and less intensive care utilization.5,6
Practically, health care providers should take some steps to show compassion: (1) emotional presence, (2) entering the patient’s world, (3) effective communication, (4) displaying understanding and kindness, and (5) taking practical steps to help them in their suffering.
While caring for patients, focusing on human connection is the key to forming a good relationship. Expressing compassion while caring for patients makes them feel more comfortable discussing what they are experiencing. It ultimately builds a relationship that is based on trust.
LAW OF COMMUNICATION
Also critical to connecting with patients is effective communication, which includes four key elements (Figure 2):
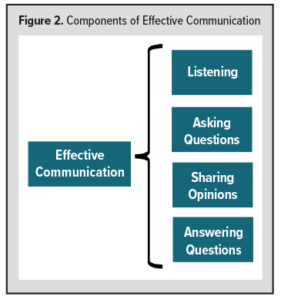 Listening: Listening is essential for any communication. There’s an old saying: “Fifty percent of medical problems would be cured if your physician just listened to your problems.” The principles of effective listening to patients are:
Listening: Listening is essential for any communication. There’s an old saying: “Fifty percent of medical problems would be cured if your physician just listened to your problems.” The principles of effective listening to patients are:
- Listen with ears open.
- Understand each word.
- Understand the meaning of each word.
- Understand the meaning between the lines.
- Understand body language.
- Avoid multitasking while listening.
- Avoid interruptions.
By following these principles, our patients understand that we care and understand their concerns.
Asking questions: Asking questions to better understand the patient’s issues is also essential to communication. Asking questions can help clinicians to dig deeper and learn more about any problems. Further, asking questions helps patients understand that their clinician has a genuine concern for their medical issues.
Sharing opinions: Sharing expert and honest opinions with patients helps the clinician to strengthen their connection. Detailed medical information should be communicated understandably to patients. Outstanding clinicians use paper and pen or whiteboards to discuss complex medical issues, and they should share the logic behind their decisions and the possible outcomes of those decisions.
Answering questions: Another critical component of communication with patients is giving them time to think through the issue, after which clinicians should make themselves available to answer any questions. It’s important to remember that all questions are valid. Patients should be encouraged to ask anything, no matter how minor or straightforward it may seem. Making patients feel comfortable and answering their questions helps them develop confidence in their clinician.
LAW OF SHARED DECISION-MAKING
Shared decision-making is a process in which the health care provider and patient work together to make the best decision for that patient, and it is a crucial component of connecting with patients. Difficult medical decisions are more manageable when the patient understands the problem and shares in the decision-making. It’s human nature to accept the decisions in which we have ownership.
A detailed account of shared decision-making is given in a previous editorial.7 In short, shared decision-making is critical for creating genuine clinician-patient relationships and is associated with better patient outcomes and satisfaction.
To develop shared decision-making, I proposed the 4C model (Figure 3):
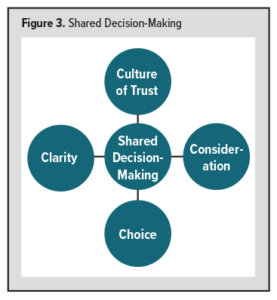 Step 1: Develop a Culture of Trust: With integrity, compassion, kindness, and humility, physicians develop a relationship of trust with their patients. In this culture of faith, a difficult decision can be made quickly.
Step 1: Develop a Culture of Trust: With integrity, compassion, kindness, and humility, physicians develop a relationship of trust with their patients. In this culture of faith, a difficult decision can be made quickly.
Step 2: Bringing Clarity: Adding clarity to the patient’s challenging medical issues always makes it easier for them to understand their medical problems and share in decision-making.
Step 3: Consideration: After better understanding the medical issues, physicians should explain all the possible treatment options, including the pros and cons of each.
Step 4: Choice: Finally, with a better understanding of the medical issues and possible treatment options, patients should be encouraged to make their decision. Ownership of the decision leads to better adherence to the treatment plan.
LAW OF HOPE
“Hope is life.” Hope is essential to a patient’s quality of life. It is well-known that people with higher hope show better adaptation, lower stress levels, and less anxiety and depression. While clinicians must be honest with their patients, they should also try to convey any “silver linings” in difficult situations. Doing so can help patients find hope and strengthen their relationship with their clinician.
Feelings of being alone in the situation, persistent pain, lack of sleep, and reduced self-esteem have a negative impact on hope. An empathetic dialogue with the patient – with a clear message from the clinician – leaves room for hope, which helps the patient heal more quickly and better connect with their clinician.
The primary sources of hope for patients include the following:
- their close relationship with their physician.
- better communication and connection with their clinician.
- a sense of self-worth.
- a positively assessed life.
- possibility of meaningful life goals.
- spiritual support.
A clinician’s positive attitude toward their patients is contagious; miracles can happen with hope.
CONCLUSION
By following these four essential laws of connection – compassion, communication, shared decision-making, and hope – we can become connecting clinicians. It is crucial that we put extra effort into incorporating these laws in our daily practice to establish lifelong relationships with our patients.
REFERENCES
- Bloom P. Empathy and its discontents. Trends Cogn Sci. 2017;21(1):24-31. doi: 10.1016/j.tics.2016.11.004
- Kirby JN. Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychol Psychother. 2017;90(3):432-455. doi:10.1111/papt.12104
- Strauss C, Lever Taylor B, Gu J, et al. What is compassion and how can we measure it? A review of definitions and measures. Clin Psychol Rev. 2016;47:15-27. doi:10.1016/j.cpr.2016.05.004
- Doohan I, Saveman BI. Need for compassion in prehospital and emergency care: a qualitative study on bus crash survivors’ experiences. Int Emerg Nurs. 2015;23(2):115-119. doi:10.1016/j.ienj.2014.08.008
- van der Cingel M. Compassion in care: a qualitative study of older people with a chronic disease and nurses. Nurs Ethics. 2011;18(5):672-685. doi:10.1177/0969733011403556
- Lown BA, Muncer SJ, Chadwick R. Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Educ Couns. 2015;98(8):1005-1010. doi:10.1016/j.pec.2015.03.019
- Aziz F. The power of shared decision-making in medical settings. WMJ. 2023;122(1):5-6.