Veronika Mak, MSc; Julia Schiller, PT, DPT; Alina Grimaldo; Ellen N. Sutter, PhD, PT, DPT; Kellie M. Collins, PT, DPT; Bernadette T. Gillick, PhD, MSPT, PT
WMJ. 2024;123(6):625-626.
In medical research, establishing partnerships among clinicians, researchers, and participants can be facilitated by effective communication and collaboration. This synergy becomes critical when considering vulnerable populations, such as children and their families. The nuances of communication and collaboration play a pivotal role in ensuring the ethical and respectful inclusion these groups in research endeavors.
Family-centered care, shared decision-making, transdisciplinary collaboration, and culturally responsive practices can be incorporated within research design and recruitment retention efforts. These techniques influence successful engagement and optimize the overall research participation experience for all involved, exemplifying how to conduct ethically sound and impactful medical research with vulnerable populations.
Current best practices recommend a heightened emphasis on advancing pediatric research through a collaborative approach that actively involves families. There is a shift from merely conducting research on children to working with children in research as they are integral to the outcomes. Several strategies facilitate this shift, including promoting diversity, equity, and inclusion initiatives; considering social determinants of health; creating community advisory boards; using face-to-face recruiting and financial incentives; and increasing parent and child engagement throughout the study.1 These methods have proven effective in recruiting and retaining families in pediatric medical research, with the latter emerging as one of the most effective strategies recommended by families and researchers.2 Consequently, prioritizing meaningful and educational engagement with families and children is a crucial focus for our research teams, aiming to enhance families’ understanding of their participation in research.
The Pediatric Neuromodulation Lab at the Waisman Center of the University of Wisconsin-Madison is currently conducting a longitudinal observational study exploring the impact of perinatal brain injury on motor development and risk for cerebral palsy (NIH-1R01HD098202). Following consultations with medical professionals, discussions with families of past participants, and relevant literature on perinatal brain injury, the research team recognized that families may have complex emotions regarding research participation based on their experiences while navigating their child’s health care needs. Respecting the families’ journey, we aim to facilitate communication between the research team and participating family. Knowledge of families’ experiences and research indicating that families prefer active engagement with research teams prompted the lab to create a “Travel Passport.” This tool guides families throughout each of the study visits in their research journey over the first 2 years of their child’s life.
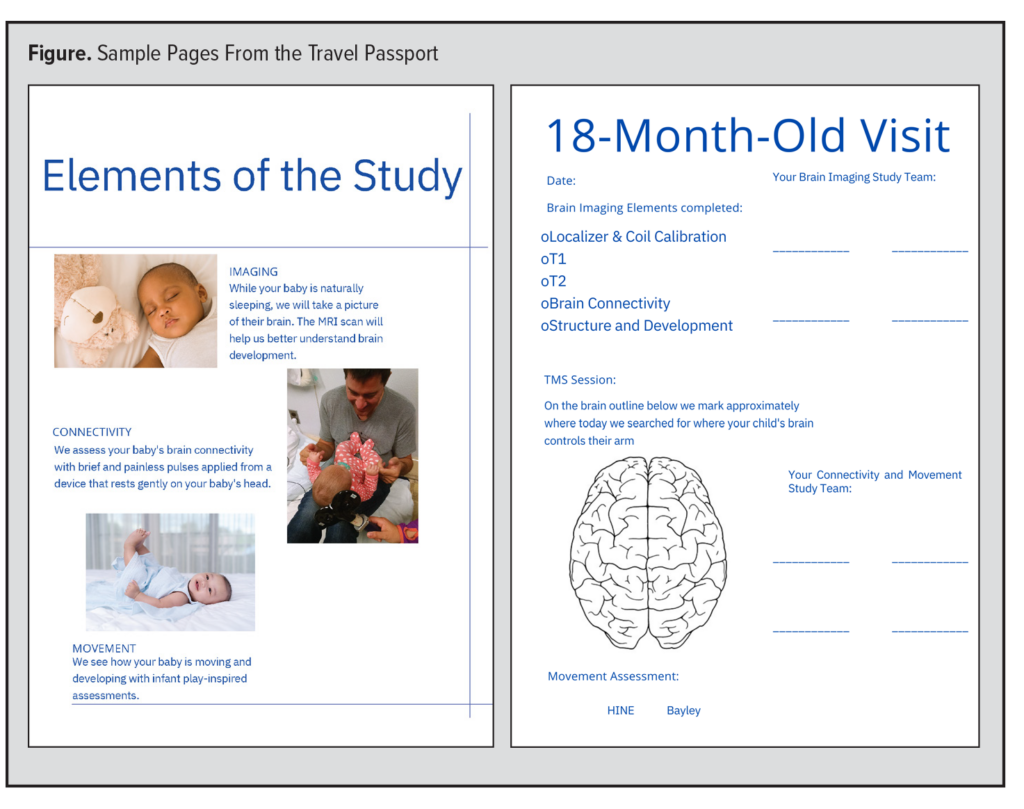 The Travel Passport aims to provide easily understandable information about the study, individualized detail of each assessment, and a tangible tool for tracking and documenting participation before the publication of results. On the first day of study participation, each family receives a customized passport packet. After each visit, they receive a “stamp” and summaries detailing the activities their child completed during their visit. Each study visit includes several different research assessments, and the Travel Passport describes each element in plain language, with a calculated Flesch-Kincaid readability score at approximately a 10th grade reading level. Additionally, the Travel Passport includes pictures and names of the individuals involved in the study and positions the family as the “center” of the research team to highlight that their involvement remains at the core of our work. The Passport remains with the family, allowing them to take it home for their reference.
The Travel Passport aims to provide easily understandable information about the study, individualized detail of each assessment, and a tangible tool for tracking and documenting participation before the publication of results. On the first day of study participation, each family receives a customized passport packet. After each visit, they receive a “stamp” and summaries detailing the activities their child completed during their visit. Each study visit includes several different research assessments, and the Travel Passport describes each element in plain language, with a calculated Flesch-Kincaid readability score at approximately a 10th grade reading level. Additionally, the Travel Passport includes pictures and names of the individuals involved in the study and positions the family as the “center” of the research team to highlight that their involvement remains at the core of our work. The Passport remains with the family, allowing them to take it home for their reference.
To evaluate the effectiveness and impact of the Travel Passport, the Pediatric Neuromodulation Lab actively seeks feedback from families, clinicians, and researchers. Through a short, anonymous survey, families provide feedback after their study visits. Survey questions cover perceptions and use of the passport, suggestions for improvement, and likes and dislikes. Eleven of the 16 families involved in the study who received a Travel Passport provided input. Eight of the 11 respondents found the Travel Passport “helpful” or “very helpful” in explaining their child’s participation in the study. Additionally, 82% of families expressed either having used or intending to use the Travel Passport to describe their experiences in the study to family, friends, or their children. Favorite components of the Passport included reference materials, the ability to track visits and development, and the inclusion of team pictures. One parent noted, “We found the breakdown of what was going to happen at each visit helpful. We also enjoyed the pictures of the team who helped facilitate each visit being attached to the passport.” For future improvements of the Travel Passport, respondents recommended a digital version and further descriptions of study results.
Various research team members, including the medical monitor and medical director have recognized the Travel Passport as an innovative method to engage participants in the research process. It has been presented at local and national conferences to reach a diverse audience and gather valuable feedback. The response from researchers and medical professionals has been overwhelmingly positive, with some clinicians contemplating the integration of a tool like the Travel Passport into their specialty practices. They see its potential to offer education, facilitate conversations, and track development by incorporating patients’ medical experiences.
We aim to share this tool as a catalyst for increasing science literacy, enhancing comprehension of research participation, and promoting participant engagement. To integrate families as active research team members, the Pediatric Neuromodulation Lab created the Travel Passport to facilitate meaningful involvement throughout the observational, longitudinal study. We remain committed to assessing participants’ perspectives on the passport to cultivate a collaborative and informative research environment.
REFERENCES
- Huntington C, Newton JT, Donaldson N, et al. Lessons learned on recruitment and retention in hard-to-reach families in a phase III randomised controlled trial of preparatory information for children undergoing general anaesthesia. BMC Oral Health. 2017;17(1):122. doi:10.1186/s12903-017-0411-4
- Weintraub JA, Breland CE. Challenges, benefits, and factors to enhance recruitment and inclusion of children in pediatric dental research. Int J Paediatr Dent. 2015;25(5):310-316. doi:10.1111/ipd.12176