Scott B. Reeder, MD, PhD; Robert N. Golden, MD
WMJ. 2025;124(1)78-79.
The discovery of x-rays by Wilhelm Röntgen, PhD, in 18951 launched the field of medical imaging and revolutionized medicine in ways he would never have imagined. The ways in which modern X-ray and derivative technologies like computed tomography (CT), digital subtraction angiography, and bone mineral density and other technologies such as ultrasound, magnetic resonance imaging (MRI), and positron emission tomography have transformed health care are myriad. Gone are the days of exploratory laparotomies and diagnostic burr holes for suspected epidural hematomas. Arrived is a new era of imaging-based molecular diagnosis, staging, and treatment monitoring of cancer, as well as imaging-guided therapies such as histotripsy and theranostic.
Imaging is now a fundamental technology for many key research approaches related to Alzheimer’s disease and other neurological and psychiatric diseases. Drug discovery trials increasingly use quantitative imaging as endpoints and eligibility for new, expensive drugs require imaging assessment.2 Imaging is the main portal of entry for many facets of tertiary care, whether it involves cancer, cardiovascular disease, or prenatal diagnosis of congenital heart disease. Indeed, the widely cited survey by Fuchs and Sox of physicians on the importance of medical innovations identified MRI and CT as the most impactful for patient care, ahead of angiotensin-converting enzyme inhibitors, statins, coronary bypass, and other discoveries in modern medicine.3 It is no wonder that the use of diagnostic imaging and image-guided therapies has skyrocketed in recent years. At UW Health, we expect to perform more than 1 million exams per year by the time we celebrate our Department of Radiology’s centennial anniversary in 2027.
With such utilization comes great cost in capital equipment and in the rapidly growing workforce needed to operate equipment, interpret exams, and treat patients. From a global sustainability perspective, by some estimates, health care represents 9% of carbon emissions, led by radiology with approximately 0.8% of all carbon emissions from CT and MRI alone, compared to aviation at 2.5%.4 We urgently need sustainable ways to provide imaging-based care. As stewards of these precious resources, the radiology community must rethink how we deliver imaging-based care.
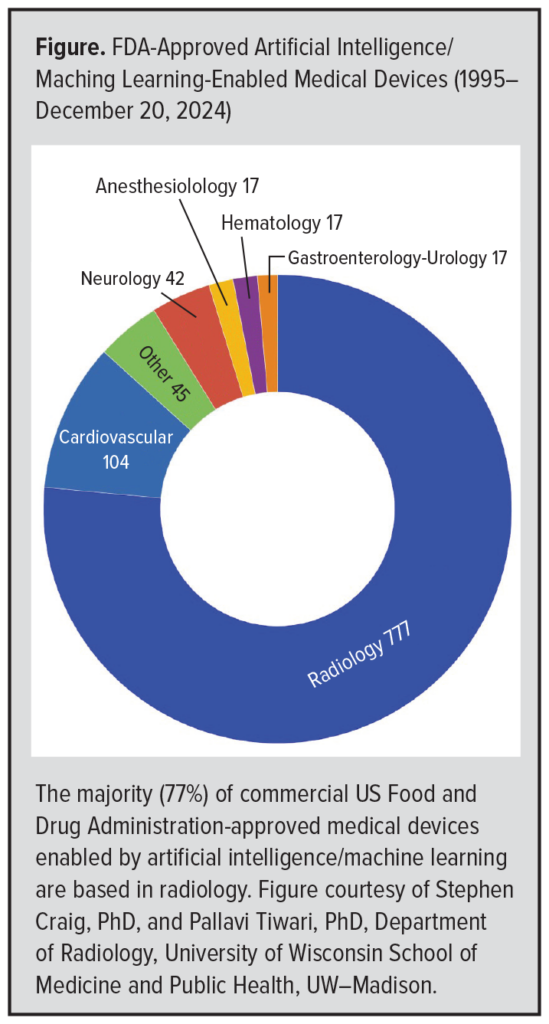 We also are witnessing a revolution through the emergence of artificial intelligence (AI)/machine learning (ML). Applications of AI have profoundly impacted all areas of medicine, but perhaps imaging has seen the greatest initial penetrance, with more than 77% of the over 1000 US Food and Drug Administration-approved AI-related technologies based in radiology (Figure).5 We view this disruption as a generational opportunity to transform imaging technologies and to “bend the curve” to ensure a sustainable future.
We also are witnessing a revolution through the emergence of artificial intelligence (AI)/machine learning (ML). Applications of AI have profoundly impacted all areas of medicine, but perhaps imaging has seen the greatest initial penetrance, with more than 77% of the over 1000 US Food and Drug Administration-approved AI-related technologies based in radiology (Figure).5 We view this disruption as a generational opportunity to transform imaging technologies and to “bend the curve” to ensure a sustainable future.
In parallel with the development of AI are new paradigms such as “opportunistic screening,” whereby actionable information can be derived from medical images to benefit patients. Perry Pickhardt, MD, a University of Wisconsin School of Medicine and Public Health (SMPH) faculty member who is a leader in this field, has led the charge using CT scans performed for other reasons (eg, abdominal pain) to derive bone mineral density, aortic calcium scoring, and body composition as biomarkers and prognostic predictors of osteoporosis, major adverse cardiac events, and cardiometabolic diseases, among others.6 Enabled by AI-based algorithms, the application of automated technologies to routine imaging exams poses a unique opportunity to increase the information content, or value, of imaging at little or no additional cost. For the first time, we also are witnessing the use of AI-based algorithms to move us toward the realization of population-based precision imaging as a cornerstone for precision health.
The confluence of economic and sustainability pressures, strains on the workforce, continued success and growth of medical imaging, and emergence of advanced analytics and disruptive AI-based technologies all converge toward a new paradigm of “high-value imaging.” We define high-value imaging as a comprehensive strategy for patient-centered imaging aimed at maximizing access, efficiency, patient experience, and actionable imaging-derived information. Developing strategies for delivering imaging care in more efficient ways is fundamental to good stewardship of important human and technological resources.
Closely related to this opportunity is the need to translate the remarkable discoveries of the University of Wisconsin–Madison and local biotechnology and medical technology (medtech) industries — such as GE HealthCare, Epic, and Exact Sciences — into widespread clinical practice. This tenet is central to the Wisconsin Idea to bring discoveries of the university to the citizens of Wisconsin and beyond, and to the principles of high-value imaging. How do we create the infrastructure and foster a mindset to accelerate discoveries in imaging into practical solutions that benefit patients everywhere?
Transforming any field involves both major challenges and enormous opportunities. This is why the SMPH and UW Health are launching the Center for High Value Imaging (CHVI), an initiative aimed at transforming the way diagnostic imaging and image-guided therapies are delivered. Through the use of data science and AI, the CHVI will bring together key stakeholders within the university and academic medical center and will partner with external collaborators to address challenges and opportunities in medical imaging. A central feature of the CHVI is the “command center” in which a nexus of analytics and real-time dashboards will enable decision-making and create a process of continuous, data-driven improvements for increased efficiency, access, and the best possible patient experience. Human factors engineering will aim to create the best working environment for professionals, maximizing their career fulfillment, reducing burnout, and maximizing their potential to the betterment of our patients. The CHVI also will create the technological and regulatory infrastructure to accelerate translation of innovations into clinical operations. In this way, “Innovation to Operations (I2O)” will be the guiding mantra of the CHVI. The unique medtech ecosystem of Wisconsin, in combination with the Isthmus Project and Wisconsin’s designation as a Regional Technology and Innovation Hub (Tech Hub), will help fully realize this vision. All of the factors will enhance the training of future generations of medical imaging engineers, technologists, radiologists, and others in related fields.
A CHVI pilot launched in 2024 has focused on MRI operations at the new Eastpark Medical Center, which opened in October 2024. Initial results have exceeded all expectations. This has been achieved through advanced analytics characterizing the utilization of MRI resources and an innovative architectural design of a “Smart Suite” pair of MRI scanners, each with two doors and two tables to optimize on-time starts and patient access. Since the beginning of the pilot, we have reduced MRI wait times to less than a week and achieved more than 50% increase in patient throughput, effectively providing the services of three MRI scanners with just two. Patient feedback has been overwhelmingly positive, and the teamwork and energy from the CHVI team has been inspiring.
Beyond the initial pilot for MRI, the CHVI will expand to all radiology subspecialities through the leadership of Dania Daye, MD, PhD, associate professor of radiology. Recently recruited from Mass General Brigham, Dr Daye is an internationally recognized leader in the use of AI-based technologies for quality and operations. She also will serve as the SMPH Department of Radiology’s vice chair for practice transformation and will lead the strategy and implementation of the CHVI, taking transformation to the national level. We welcome collaboration with stakeholders for whom medical imaging plays a role in their practice or research. Together we will expand the impact of the CHVI, most importantly maximizing patients’ access and experience, as well as the value of the lifesaving diagnostic and image-guided treatments they receive.
REFERENCES
- Röntgen WC. Über eine neue Art von Strahlen (Vorläufige Mittheilung) Sitzungsberichte der Physikalisch-medizinischen Gesellschaft zu Würzburg. 1895;29:132–141.
- Sirlin CB, Reeder SB. A new era for quantitative MRI biomarkers of the liver: a challenge and opportunity for the radiology community. Radiology. 2024;313(3):e241876. doi:10.1148/radiol.241876
- Fuchs VR, Sox HC Jr. Physicians’ views of the relative importance of thirty medical innovations. Health Aff (Millwood). 2001;20(5):30-42. doi:10.1377/hlthaff.20.5.30
- Rockall AG, Allen B, Brown MJ, et al. Sustainability in radiology: position paper and call to action from ACR, AOSR, ASR, CAR, CIR, ESR, ESRNM, ISR, IS3R, RANZCR, and RSNA. J Am Coll Radiol. 2025:S1546-1440(25)00113-9. doi:10.1016/j.jacr.2025.02.009.
- Artificial Intelligence and Machine Learning (AI/ML)-Enabled Medical Devices. US Food and Drug Administration. Reviewed March 25, 2025. Accessed March 17, 2025. https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-and-machine-learning-aiml-enabled-medical-devices
- Pickhardt PJ, Kattan MW, Lee MH, et al. Biological age model using explainable automated CT-based cardiometabolic biomarkers for phenotypic prediction of longevity. Nat Commun. 2025;16(1):1432. doi:10.1038/s41467-025-56741-w