Fahad Aziz, MD, FASN, WMJ Editor-in-Chief
WMJ. 2023;122(1):5-6.
Shared decision-making is a process where a health care provider and a patient work together to make the best decision for the patient. It is a crucial component of patient-centered health care. Sharing our expert, honest opinions with patients helps to strengthen our connection, and difficult medical decisions are more manageable when the patient fully understands the problem and shares in the decision-making. It’s our nature to accept the decisions in which we have ownership.
The patient-clinician relationship is one of the most meaningful experiences shared by humans. It’s a consensual relationship where the patient voluntarily seeks the clinician’s assistance, and the clinician knowingly accepts that person as a patient. However, this relationship can be very complicated and is not always perfect. Good patient-clinician relationships go beyond excellent bedside manner and are built on trust.
MODELS OF THE DOCTOR PATIENT RELATIONSHIP
In 1956, Szasz et al described three basic models of the doctor-patient relationship:1
- Active-passive model: This model is based on the physician acting on the patient without input. It may be appropriate during an emergency where the physician act quickly and the patient is not in a state to make any critical decisions.
- Guidance-cooperation model: In this model, the physician decides, based on their medical knowledge, what’s best for the patient. The clinician makes a recommendation, and the patient is expected to comply.
- Mutual participation model: This model is based on equal participation between the clinician and the patient and requires that both parties engage in activities that they find satisfying.
Each model has utility in specific situations; however, due to its tremendous advantages, there has been considerable support for the mutual participation model over the last few decades.
ADVANTAGES OF SHARED DECISION-MAKING
A shared decision-making approach can provide a readily understandable roadmap to keep clinicians moving toward success in clinical scenarios. It is the key to handling complex, emotion-laden situations with transparency and confidence and includes the following benefits.
A. Patient and clinician satisfaction: Giving patients a chance to describe their preferences and then helping them understand the risks and benefits of their decisions increases their satisfaction with the care they are receiving. Several studies have shown that patients who were more involved in the decisions made by their clinicians were more knowledgeable about their condition and were more satisfied with their medical care2 and clinicians feel satisfied when they provide high-quality care with the support of their patients.3
B. Better outcomes: Shared decision-making reduces patient anxiety and improves patient compliance with their treatment plan. They have more knowledge of their medical conditions and have a better understanding of the potential risks and benefits of the treatment, which plays an essential role in physicians’ job satisfaction and reduces clinician burnout.3
C. Better connection between patients and clinicians: As clinicians, we know that connecting with our patients is a powerful tool.4 Listening to the their concerns, giving them an honest opinion, and then answering their questions helps them understand the clinical situation and the risks and benefits of treatment options. Sharing in decision-making forges a strong connection between patients and clinicians and ensures the decision is one patients can own and respect.
SHARED DECISION-MAKING PROCESS
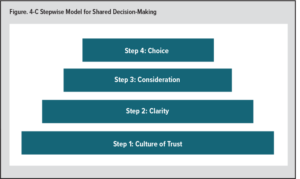
To develop a shared decision-making process, I propose the 4-C stepwise model (see Figure).
Step 1: Develop a culture of trust: In the pyramid shared decision-making, the culture of trust between a clinician and patient always comes first. Building trust takes time, and with repeated displays of their integrity, clinicians can create a relationship of trust with their patients.
Step 2: Clarity: One of the most critical components of shared decision-making is adding clarity to the situation. I have seen outstanding physicians use paper and pen or a whiteboard while discussing complex issues and possible solutions with their patients.
Complex medical problems can be made more accessible by adding clarity, which has two components:
- Listen carefully. With their busy schedules, many clinicians don’t have much time to spend with each patient, and patients too often feel rushed through their visits. Patients must not feel rushed; instead, they should be given time to share their and concerns. There is an old saying: “Fifty percent of medical problems would be cured if your physician just listened to your problems.”4
- Allow ample time for questions. Patients should be given enough time to think through the issue, and clinicians should make themselves available to answer any questions. It’s important to remember that all questions are valid, and patients should be encouraged to ask anything—no matter how minor or straightforward it may seem. Making patients feel comfortable and answering their questions helps clinicians earn their patient’s confidence—a crucial component of shared decision-making.
Step 3: Consideration: After the patient understands their medical issue(s), clinicians should explain all possible treatment options and the risks and benefits of each, and patients should be encouraged to ask questions about those treatment options.
Step 4: Choice: After understanding the process and available treatment options, patients should be encouraged to make decisions with their clinician. Ownership boosts a patient’s confidence and adherence to their treatment plan.
If we wish to be clinicians who are “connecting” and “influencing,” it’s essential that we make shared decisions with our patients—and that we teach and demonstrate the power of shared decision-making to future health care professionals.
REFERENCES
- Szasz TS, Hollender MH. A contribution to the philosophy of medicine; the basic models of the doctor-patient relationship. AMA Arch Intern Med. 1956;97(5):585-592. doi:10.1001/archinte.1956.00250230079008
- Hughes TM, Merath K, Chen Q, Sun S, Palmer E, Idrees JJ, et al. Association of shared decision-making on patient-reported health outcomes and healthcare utilization. Am J Surg. 2018;216(1):7-12. doi:10.1016/j.amjsurg.2018.01.011
- Dobler CC, West CP, Montori VM. Can shared decision making improve physician well-being and reduce burnout? Cureus. 2017;9(8):e1615. doi:10.7759/cureus.1615
- Aziz F. All clinicians communicate with patients, but too few connect. WMJ. 2022;121(3):172-173.