Fahad Aziz, MD, FASN, WMJ Editor-in-Chief
WMJ. 2023;122(3):160-161
On February 27, 2007, a crash occurred before 9 AM between two buses on a snowy road in central Sweden. In this terrible accident, at least six people died, nine were seriously injured, and 42 suffered minor injuries. Most of the wounded were taken to Uppsala University Hospital. Two of the most seriously injured were airlifted to a Stockholm hospital.1
In 2014, Doohan et al conducted telephone interviews with the survivors. The sample consisted of 54 of 56 survivors: 21 women and 33 men. The questions asked were about prehospital discomfort, lack of compassionate care, and dissatisfaction with crisis support. Even after so many years, the survivors remembered not only the physical pain but also the lack of compassion they received in the emergency department. The authors concluded that a lack of compassion among health care professionals affected the patients’ well-being to the degree that it remains one of the worst memories of the crash seven years later.2 While patients and families may not remember the name or face of a doctor or nurse who cared for them on one of the worst days of their life, the slightest compassion they receive from health care professionals may stick with them long after.
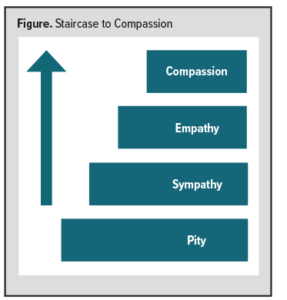 Derived from a Latin word that means “together suffering” or “fellow in feelings,” compassion arises in response to someone’s suffering and includes a motivation to relieve their suffering. And while similar to pity, sympathy, and empathy, there are clear differences. Pity is a simple expression of sorrow; sympathy goes a step further; it is composed of a range of feelings and means understanding what the other person is feeling. Finally, empathy is feeling what the other person is feeling but does not require action or sustain itself over time.3 (See Figure.)
Derived from a Latin word that means “together suffering” or “fellow in feelings,” compassion arises in response to someone’s suffering and includes a motivation to relieve their suffering. And while similar to pity, sympathy, and empathy, there are clear differences. Pity is a simple expression of sorrow; sympathy goes a step further; it is composed of a range of feelings and means understanding what the other person is feeling. Finally, empathy is feeling what the other person is feeling but does not require action or sustain itself over time.3 (See Figure.)
Physician/scientists Stephen Trzeciak and Anthony Mazzarelli wrote in their book Compassionomics, The Revolutionary Scientific Evidence That Caring Makes a Difference, “Empathy is like a one-way street running toward the health care provider: detecting, processing, understanding, and even feeling the incoming emotional cues from the patient. Compassion, on the other hand, is a street that runs in the other direction, a responsive action toward the one who is suffering. Empathy can happen through a one-way mirror. Compassion cannot.”4 In other words, compassion has two components: (1) feeling someone’s suffering, and (2) the ability to take action to relieve them from that suffering.5,6
WHY DOES COMPASSION MATTER?
Patient Outcomes
The release of Compassionomics ignited a conversation about the relationship between physician compassion and patient outcomes, and several studies have demonstrated that health care providers’ compassion significantly improved patients’ clinical outcomes – especially those with chronic medical conditions.
Watts et al aimed to elucidate the role of compassionate care in various aspects of medicine and health care delivery. They conducted a literature review of four databases and included 22 articles in the study. Their analysis showed that along with enhanced patient outcomes, compassionate care was associated with reduced care costs, lower rates of compassion fatigue and burnout, and fewer malpractice claims.7
In another study, Hojat et al tested the hypothesis that health care compassion is associated with favorable clinical outcomes in diabetic patients. The study included 891 diabetic patients and showed that patients of physicians with high empathy scores were significantly more likely to have reasonable control of their hemoglobin A1c (56%) than were patients of physicians with low empathy scores (40%, P < .001). The study concluded that health care providers’ compassion is an essential factor associated with better clinical outcomes in patients with diabetes.8 Several other studies showed that compassionate care by physicians, physician assistants, and nurses predicts faster recovery, significant autonomy, lower intensive care utilization, and more responsible healthcare management.9-12
The above data showed that the healthcare provider’s compassion significantly improved patients’ clinical outcomes, especially those with chronic medical conditions.
Clinician Burnout
In their 2022 book Wonder Drug: 7 Scientifically Proven Ways That Serving Others Is the Best Medicine for Yourself, Trzeciak and Mazzarelli demonstrate that providing compassionate care to patients is extremely important for health care providers. It prevents burnout and compassion fatigue and is also a source of happiness and accomplishment.13 “You don’t lose anything by serving others, you only gain. Giving is a powerful therapy for the giver, any giver,” said Trzeciak.
COMPONENTS OF COMPASSIONATE CARE
There are three essential components of companionate care:
- Serve by intention: In the words of leadership expert and author John C. Maxwell, “Good intentions turn into good actions.” A genuine intention to help people in their suffering is the most essential and crucial step to compassionate care.
- Be humble: Humility and gratitude are also crucial to compassionate care. In his interview with Oprah Winfrey in 2001, Nelson Mandela said, “Humility is the most important thing you should have to succeed. If you make people realize you are no threat to them, they will take no time to embrace you.” Being a humble and grateful health care professional does not equal weakness or being soft; rather, it reduces arrogance and strengthens the clinician.
- Spread hope: Believing is a significant factor in a patient’s recovery.13 Spreading hope does not mean giving false information but rather showing “silver linings” in difficult medical conditions. When a patient has hope, it can have a positive impact on their quality of life, leading to better adaptation and lower stress levels, anxiety, and depression.
American author John Nasibitt once said, “The most exciting breakthroughs of the 21st century will not occur because of technology, but because of an expanding concept of what it means to be human.”
With the pressures we face as clinicians every day, providing compassionate care is essential. Not only does it produce better clinical outcomes for patients, but it is a defense against burnout. Unfortunately, in conventional medical education, the importance of compassionate care is rarely taught. It is crucial that we put extra effort into incorporating “compassionate care” teaching into the curriculum of our future medical providers.
REFERENCES
- Nordstrom L. Bus collision kills 6, injures nearly 50 in Sweden. Associated Press. February 27, 2007. https://www.chron.com/news/nation-world/article/Bus-collision-kills-6-injures-nearly-50-in-Sweden-1533717.php. Accessed June 15, 2023.
- Doohan I, Saveman BI. Need for compassion in prehospital and emergency care: a qualitative study on bus crash survivors’ experiences. Int Emerg Nurs. 2015;23(2):115-119. doi:10.1016/j.ienj.2014.08.008
- Bloom P. Empathy and its discontents. Trends Cogn Sci. 2017;21(1):24-31. doi:10.1016/j.tics.2016.11.004.
- Trzeciak S, Anthony M. Compassionomics: The Revolutionary Scientific Evidence that Caring Makes a Difference. Studer Group. Kindle Edition; 2019.
- Kirby JN. Compassion interventions: The programmes, the evidence, and implications for research and practice. Psychol Psychother. 2017;90(3):432-455. doi: 10.1111/papt.12104
- Strauss C, Lever Taylor B, Gu J, et al. What is compassion and how can we measure it? A review of definitions and measures. Clin Psychol Rev. 2016;47:15-27. doi:10.1016/j.cpr.2016.05.004
- Watts E, Patel H, Kostov A, Kim J, Elkbuli A. The role of compassionate care in medicine: toward improving patients’ quality of care and satisfaction. J Surg Res. 2023;289:1-7. doi:10.1016/j.jss.2023.03.024
- Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. doi:10.1097/ACM.0b013e3182086fe1
- Spandler H, Stickley T. No hope without compassion: the importance of compassion in recovery-focused mental health services. J Ment Health. 2011;20(6):555-566. doi: 0.3109/09638237.2011.583949
- Sharp S, McAllister M, Broadbent M. The vital blend of clinical competence and compassion: How patients experience person-centred care. Contemp Nurse. 2016;52(2-3):300-312. doi:10.1080/10376178.2015.1020981
- Lown BA, Muncer SJ, Chadwick R. Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Educ Couns. 2015;98(8):1005-1010. doi:10.1016/j.pec.2015.03.019
- van der Cingel M. Compassion in care: a qualitative study of older people with a chronic disease and nurses. Nurs Ethics. 2011;18(5):672-685. doi:10.1177/0969733011403556
- Trzeciak S MA. Wonder Drug: 7 Scientifically Proven Ways That Serving Others Is the Best Medicine for Yourself. St. Martin’s Publishing Group. Kindle Edition; 2022.